Our Services
Assess foot and leg movement to find pain causes. Bring footwear and wear loose clothing. Biomechanical Assessment
Assess and treat sports-related foot and leg injuries to improve movement and performance. Sports Podiatry Analysis.
Check circulation, sensation, and pressure to detect issues early and prevent complications. Diabetic Check
Check skin and nail health, corns, calluses, and infections to guide early, personalised care. General Consultation
Biomechanical Assessment
A biomechanical assessment evaluates the structure and function of your feet, ankles, and lower limbs to identify any alignment or movement issues that may be contributing to pain or injury. Using a combination of visual analysis, gait observation, and pressure mapping (if required), we can pinpoint the root cause of discomfort and develop a personalised treatment plan. This may include orthotics, exercise programs, or other interventions designed to improve movement efficiency and reduce strain.
For the assessment bring footwear and wear shorts or loose-fitting clothing to allow for comfortable movement and an accurate assessment.
Sports Podiatry Analysis
A Sports Podiatry consultation is designed for athletes and active individuals who want to optimise performance, prevent injury, or recover from sports-related foot, ankle, or lower limb problems. During the consultation, we assess your biomechanics, movement patterns, footwear, and training techniques to identify factors that may be contributing to pain, discomfort, or reduced performance. Whether you’re an elite competitor, weekend warrior, or just enjoy staying active, our goal is to help you move efficiently, safely, and with confidence. The assessment may include gait analysis, muscle testing, and functional movement evaluation, allowing us to develop a personalised treatment plan tailored to your sport and activity level. This can include advice on footwear, strengthening exercises, and targeted interventions.
Please bring footwear and wear shorts or loose-fitting clothing to allow for comfortable movement and an accurate assessment.
Diabetic Check
A Diabetic Foot Check helps prevent long-term complications and supports overall foot health. Our comprehensive assessment includes Doppler blood flow analysis to ensure circulation is adequate, pressure plate analysis to identify high-pressure areas that could develop ulcerations, and monofilament testing to confirm protective sensation is maintained. We identify risks early, monitor circulation and sensation, and provide personalised advice to keep you active and comfortable.
Please bring your usual footwear to a diabetic check.
General Consultation
A comprehensive assessment of your feet, focusing on overall foot health, skin, and nails. During this consultation, check for any signs of abnormal pressure areas, and assess your skin and nail health, including detecting infections, thickened or discolored nails, corns, calluses, fungal conditions, and other dermatological issues that may affect your comfort and mobility.
The consultation also includes advice on preventative care, footwear selection, and strategies to reduce the risk of injury or long-term foot problems. Any findings are discussed in detail, and a personalised care plan or treatment options are provided to address existing concerns and maintain optimal foot health. This thorough evaluation ensures both immediate issues and potential future complications are identified and managed effectively.
Please bring your usual footwear to a general consutlation.
Orthotics
A biomechanical/orthotic assessment evaluates the structure and function of your feet, ankles, and lower limbs to identify alignment or movement issues contributing to pain or injury. Using visual analysis, gait observation, and pressure mapping when required, we pinpoint the root causes of discomfort and create a personalised treatment plan. This may include new orthotics, exercise programs, or other interventions designed to improve movement efficiency, reduce strain, and enhance comfort. Sometimes existing orthotics can be modified rather than remade. Assessments are tailored for everyday activity or sports performance.
Please bring your usual footwear, any older orthotics you may have, and wear shorts or loose-fitting clothing to allow comfortable movement and ensure an accurate evaluation.
If you require an orthoitc assessment please book a biomechanical assessment.
Childrens Feet
Children’s feet develop rapidly, and subtle issues in growth, posture, or movement can sometimes go unnoticed. Early assessment is important to ensure healthy foot development and to identify problems such as flat feet, in-toeing, out-toeing, or poor walking patterns before they cause discomfort or affect activity levels.
A biomechanical assessment provides a detailed understanding of how your child’s feet, legs, and body move during standing and walking. This helps detect and treat imbalances, muscle weaknesses, or alignment concerns that may contribute to pain, tripping, or fatigue.
For the assessment bring footwear and wear shorts or loose-fitting clothing to allow for comfortable movement and an accurate assessment.
If your child requires an assessment please book a biomechanical assessment.
Radial Shockwave
Radial Extracorporeal Shockwave Therapy (RSWT) is a non-invasive treatment used to relieve chronic musculoskeletal pain and promote natural healing. It is highly effective for conditions such as Achilles tendinopathy, plantar fasciitis, and other soft tissue or joint disorders affecting the foot and lower limb.
During treatment, controlled acoustic waves are delivered to the affected area, stimulating the body’s healing response. This enhances blood flow, reduces inflammation and calcium deposits, and provides a natural analgesic effect — helping to relieve pain, restore normal function, and support long-term recovery.
For shockwave therapy please book a biomechanical assessment.
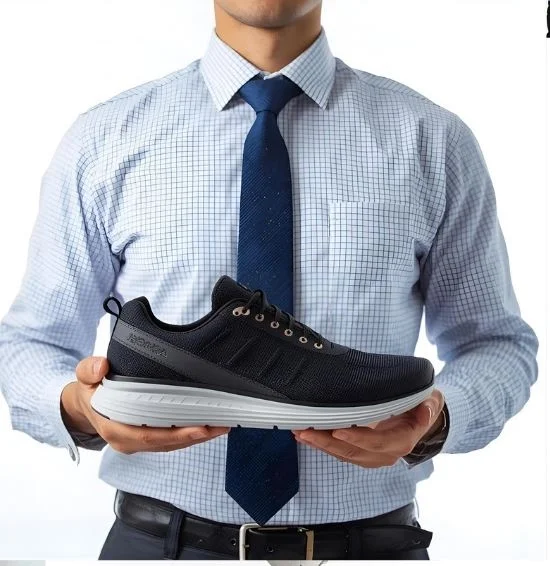
Footwear Advice
Our podiatrists provide expert guidance on selecting the right athletic footwear to match your foot type, activity level, and performance goals. The right shoes can improve comfort, enhance efficiency, and help prevent injuries during sport or exercise. We assess your foot structure, gait, and biomechanics to recommend footwear that supports optimal alignment and function. Whether you’re a runner, walker, or gym enthusiast, we’ll help you choose footwear that keeps you moving comfortably and confidently.
If you require a footwear assessment and advice please book a biomechanical assessment.
CAM Walker / Moon Boot
A CAM walker is a supportive boot used to protect and offload the foot and ankle during recovery from stress fractures, soft-tissue injuries, and post-surgical healing. At Tim Pain Podiatry, we assess your injury, ensure the boot is correctly fitted, and guide you on safe weight-bearing to reduce pain and support proper healing. We carry all sizes of CAM walkers on-site, ready for immediate fitting, along with gait advice and a tailored return-to-activity plan.
Before your appointment: wear loose clothing around the lower leg, bring any imaging or referrals, and wear supportive footwear on the non-injured side to help maintain balance and alignment.
For a CAM walker please book a biomechanical assessment.